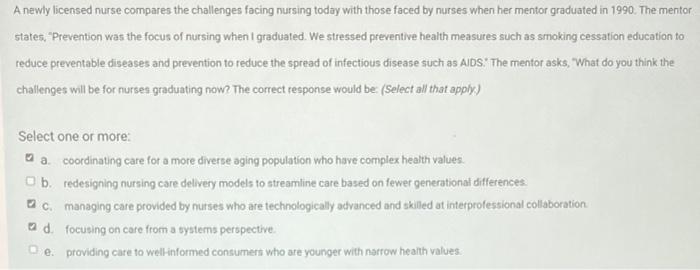
A nurse is orienting a newly licensed nurse about documentation, an essential aspect of nursing practice that ensures accurate and timely communication of patient information. This comprehensive guide will delve into the principles, types, and methods of nursing documentation, emphasizing its legal and ethical implications.
By understanding the significance of proper documentation, newly licensed nurses can enhance patient care and contribute to effective healthcare delivery.
Documentation Principles and Guidelines
Accurate and complete documentation is essential in nursing practice. It serves as a legal record of patient care, facilitates communication among healthcare providers, and supports quality improvement initiatives. Nurses must adhere to established documentation standards and guidelines to ensure the accuracy, completeness, and timeliness of their documentation.
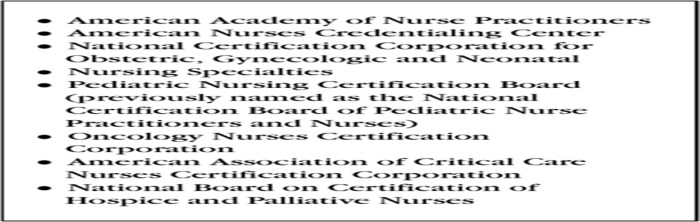
Documentation standards and guidelines vary across healthcare organizations and jurisdictions. Common standards include the Joint Commission’s National Patient Safety Goals, the American Nurses Association’s Code of Ethics for Nurses, and state nursing practice acts. These standards Artikel specific requirements for documentation, such as the use of standardized terminology, the inclusion of objective and subjective data, and the timely completion of documentation.
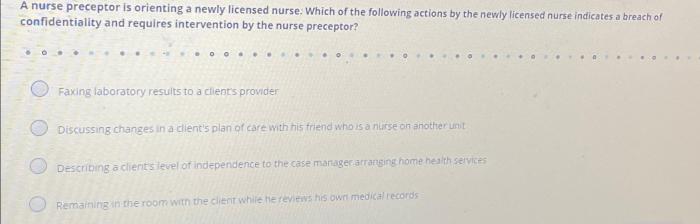
Proper documentation has legal and ethical implications. Accurate and complete documentation can protect nurses from liability by providing a record of the care they provided. Conversely, inadequate or inaccurate documentation can be used as evidence of negligence or malpractice. Nurses have an ethical obligation to document patient care accurately and completely to ensure the safety and well-being of their patients.
Types of Nursing Documentation
There are various types of nursing documentation used in clinical practice, each serving a specific purpose and containing different information.
- Progress notesdocument the patient’s condition, response to treatment, and progress over time. They typically include subjective and objective data, nursing interventions, and patient education provided.
- Medication administration recordsdocument the medications administered to the patient, including the name, dosage, route, time, and any adverse reactions.
- Discharge summariessummarize the patient’s hospital stay, including the reason for admission, diagnosis, treatment plan, and discharge instructions.
Other types of nursing documentation include intake and output records, vital sign sheets, and procedure notes. The specific types of documentation used will vary depending on the patient’s condition and the setting in which care is provided.
Subjective and Objective Data

Nursing documentation includes both subjective and objective data. Subjective data is information that is reported by the patient and cannot be objectively verified, such as pain, nausea, or anxiety. Objective data is information that can be observed or measured, such as vital signs, physical examination findings, and laboratory results.
It is important to document both subjective and objective data to provide a comprehensive assessment of the patient’s condition. Subjective data helps to understand the patient’s experience of their illness and how it affects their quality of life. Objective data provides a more concrete and measurable picture of the patient’s health status.
Charting Methods
Nurses use various charting methods to document patient care, each with its own advantages and disadvantages.
- SOAP(Subjective, Objective, Assessment, Plan) is a structured charting method that organizes documentation into four sections: subjective data, objective data, assessment, and plan.
- DAR(Data, Action, Response) is a simpler charting method that focuses on documenting the data collected, the actions taken, and the patient’s response.
- PIE(Problem, Intervention, Evaluation) is a charting method that emphasizes the identification of patient problems, the interventions implemented to address those problems, and the evaluation of the effectiveness of those interventions.
The choice of charting method depends on the patient’s condition, the setting in which care is provided, and the nurse’s preference.
Documentation of Medications and Treatments
Accurate and complete documentation of medications and treatments is essential for ensuring patient safety. Nurses must document the name, dosage, route, time, and any adverse reactions for all medications administered to the patient.
Documentation of treatments should include the type of treatment, the date and time it was performed, and the patient’s response. Nurses should also document any complications or adverse events that occur during or after treatment.
Documentation of Patient Education: A Nurse Is Orienting A Newly Licensed Nurse About Documentation
Nurses play a vital role in providing patient education. Documentation of patient education is important to ensure that the patient understands and agrees with the treatment plan and to track the patient’s progress.
Nurses should document the topics discussed with the patient, the materials provided, and the patient’s understanding of the information. This documentation can be included in the patient’s progress notes or in a separate patient education record.
Q&A
What are the key principles of nursing documentation?
Accuracy, completeness, timeliness, objectivity, and confidentiality.
What are the different types of nursing documentation?
Progress notes, medication administration records, discharge summaries, and patient education materials.
What is the difference between subjective and objective data in nursing documentation?
Subjective data is what the patient reports, while objective data is what the nurse observes.
What are the advantages of using electronic health records (EHRs) for documentation?
Improved accuracy, efficiency, accessibility, and communication.
What is the nurse’s role in patient education documentation?
To document the content of the education provided, the patient’s understanding, and any resources provided.